Clinical Decision Support
Expressing and sharing computerized clinical decision support (CDS) content across languages and technical platforms has been an evasive goal for a long time. Lack of commonly shared clinical information models and flexible support for various terminology resources have been identified as two main challenges for sharing detailed clinical rules between sites.
Clinical practice guidelines (CPG) are statements that have been systematically developed to assist practitioners (and patients) in making appropriate decisions about healthcare under specific clinical circumstances. They are generally the result of months, sometimes decades, of observational and/or interventional studies on large population groups that share certain characteristics. Sometimes, such CPGs offer assistance on when and what diagnostic or screening tests should be performed, treatment modalities to be used and other details of clinical practice.
The overarching desire is to contribute to the improvement of healthcare quality. Because of the vast number of potential clinical scenarios, CPG:s are prone to rapid change and quickly become outdated and/or too voluminous in both content and format, and difficult to consult in real-time. In an attempt to target these issues, computerized clinical decision support applications have been developed and integrated into the clinical workflow process – these applications can analyze healthcare data at the point of care, thus delivering timely, accurate, guideline-based, and personalized recommendations that enhance the overall health of patients and improve the quality and efficiency of healthcare. These applications are referred to as computerized clinical decision support systems (CDSS).
Guideline Definition Language
Cambio Healthcare Systems partnered with the openEHR Foundation to develop the formal Guideline Definition Language (GDL) that relies on openEHR archetypes and templates to represent clinical knowledge (clinical practice guidelines) for computerized clinical decision support. Discrete GDL rules can be combined into one GDL formatted (and computer processable) document and provide the logic for various types of complex decision-making based on existing practice guideline information. Such a GDL-based CDSS requires as input: the relevant patient data (in the form of archetypes and templates) as well as the relevant practice guideline information (already pre-configured); the output is then the guideline-recommended test, drug, procedure, referral, or other clinical practice detail.
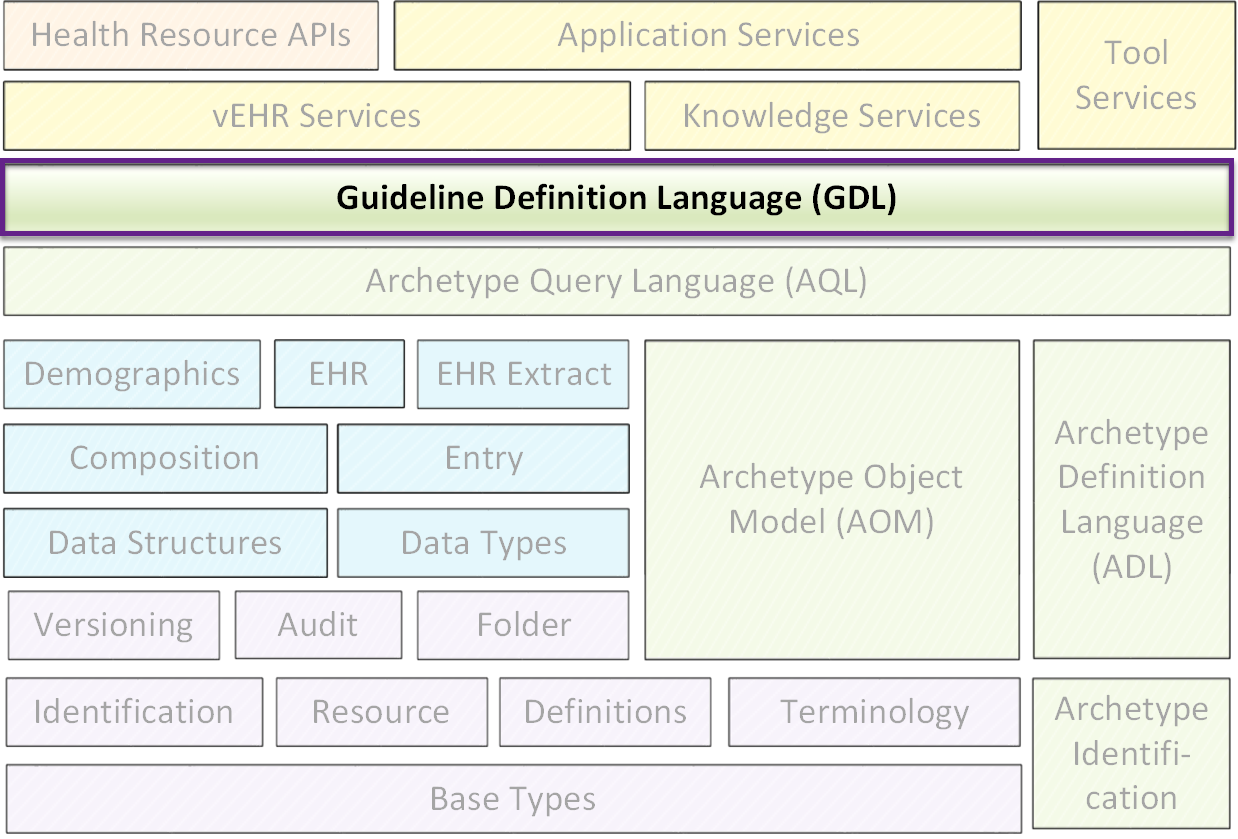
Due to the robust nature of the GDL, when practice guidelines change or are updated all that is required is a simple modification of the GDL rules that govern how the CDSS interprets the patient data, with little or no additional effort from the clinician or CDSS user. GDL and its resultant guidelines are built to be natural language- and reference terminology-agnostic as well as platform-independent, and thus semantically interoperable.
GDL 2
The second generation of the Guideline Definition Language – GDL 2 – is currently under development. After more than four years of designing and implementing CDS applications into electronic healthcare records (EHR), the time has come to increase the modelling capacity of GDL by enabling support for other standardized EHR models in addition to openEHR archetypes and templates. Thus, the scope for GDL 2 is to add native support for FHIR (Fast Healthcare Interoperabiliy Resources), develop and implement novel features and increase overall language flexibility to further expand the possibilities of clinical modelling using GDL.